Results from a large national study performed in the 1960s indicated that a number of nongenetic factors can affect the risk of ADHD. The children evaluated in that study were followed from conception until 7 years of age. Risk factors for ADHD included a history of smoking, alcohol use, drug use or anemia during pregnancy, breech birth, chorioamnionitis (infection of the placenta) during labor, premature birth, and small head size at birth. A family history of mental retardation and low socioeconomic status also appeared to be risk factors. Neurological problems in the first month of life increase the risk of ADHD at age 7 years from 2% to 50%. In infancy, delayed development and increased activity predict ADHD at age 7 years.When a 4-yearold child has a small head size, astigmatism, or visual motor, fine motor, or gross motor deficits, the risk of ADHD is increased.
Psychosocial problems at home are also risk factors for ADHD. A Hawaiian study revealed a 200% to 400% increased risk of ADHD in children from families where there was a lot of conflict in the home. In a Swedish study, unsatisfactory family life was the largest risk factor for ADHD, overriding any other medical problems.
Having a risk factor or even several risk factors does not mean that ADHD is going to occur, but it makes ADHD more likely than in someone who has no risk factors. The various risk factors predispose a child to ADHD to different degrees.
Saturday, April 30, 2011
Friday, April 29, 2011
If I have ADHD, will my child also have it?
No, not necessarily, but the chance is definitely greater than if you did not have ADHD. For example, onethird of fathers with a history of ADHD in childhood have a child with ADHD. For mothers, the percentage is somewhat lower. Sometimes, it is a male relative in the mother’s family who has ADHD. Mothers presumably have the ADHD gene, but they may exhibit few or no symptoms. Nonetheless, these mothers can pass the ADHD gene on to their children.We are still not sure why females are less likely to have ADHD symptoms, even when it is almost certain they have one of the ADHD genes. In one study of ADHD adults and controls, 43% of children with ADHD parents met criteria for a diagnosis of ADHD, compared to 2% of children in the control group of children who had parents without ADHD. If your first child has ADHD, the risk of your second child having ADHD is probably higher than in the general population. However, predicting the severity of ADHD or the type of ADHD that might run in a family is not possible.
Thursday, April 28, 2011
What causes ADHD?
By far, the most common cause of ADHD is a genetic proclivity (i.e., ADHD is often inherited). Studies suggest that the heritability rate of ADHD ranges from 0.75 to 0.91. The heritability rate indicates the percentage of ADHD in an individual resulting from genetic rather than environmental factors. Thus, a heritability rate of 0.75 means that 75% of the cause of ADHD is genetic.However, ADHD can also be caused or exacerbated by other factors, such as preterm birth, anemia, medications for asthma, and other environmental factors.
Wednesday, April 27, 2011
Would I know any famous people who have or have had ADHD?
Most certainly ADHD has affected the lives of all kinds of people including authors, inventors, military leaders, statesmen, composers, athletes, and actors and actresses. The following list includes individuals who may or may not have had diagnosed ADHD but who most certainly exhibited behavior that indicates the possible presence of ADHD or other learning disabilities. For example, Danny Glover, Bill Cosby,Tom Cruise, Jim Carrey, Robin Williams, Nolan Ryan, Jason Kidd, and Magic Johnson are all individuals who have been described as having ADHD symptoms. Many very successful entrepreneurs, such as Walt Disney and Malcolm Forbes, have also proved that their ability to “think outside the box” was perhaps a more positive consequence of ADHD. In fact, many individuals who have excelled at multitasking may have been using features of their ADHD in a positive way; their difficulties in focusing on a single task improved their ability to handle many tasks at once.
Tuesday, April 26, 2011
Does having ADHD mean that something is fundamentally wrong with my child’s brain?
ADHD is a biological, brain-based problem, but that’s not the same as saying that something is wrong with your child’s brain. There’s a big difference between damage and dysfunction. Damage causes problems with the “hardware” or the basic brain structures. That’s not what happens in ADHD. Although research data show that some brain structures, particularly the caudate, the corpus callosum (which allows the two hemispheres to “talk” to each other), and the cerebellum may be smaller in children with ADHD, but there is no indication that damage per se is present. In ADHD, the primary problem is with the “software”: the wiring or the connections in the brain. The problem with the connections most likely can be traced to atypical amounts of specific neurotransmitters, either individually or in relation to one another.
One recent imaging study showed that children with ADHD have relative cortical thinning in regions important for attention. Children with persistent ADHD had “fixed” thinning of areas of the frontal cortex, which may compromise the maturation of attentional systems. On the other hand, cortical thickness normalized in children who “outgrow” their ADHD.
One recent imaging study showed that children with ADHD have relative cortical thinning in regions important for attention. Children with persistent ADHD had “fixed” thinning of areas of the frontal cortex, which may compromise the maturation of attentional systems. On the other hand, cortical thickness normalized in children who “outgrow” their ADHD.
Monday, April 25, 2011
What genes are involved in ADHD?
You may be aware that many functions in our body, including production of hormones and other body and brain chemicals, are controlled by specific genes—the molecules of DNA that tell our cells how to develop and behave. You may not, however, have a clear idea of how this really works, and the fact is that scientists did not either until fairly recently. Mapping the human genome has helped determine some of the genes controlling specific functions, but many genes affect body systems in ways that scientists have yet to figure out. In some cases, multiple genes may be involved in complex interactions to cause an organ or a system to function properly (or improperly, as in the case of ADHD and many other disorders).
Genetic studies of ADHD have focused largely on genes involved in controlling the neurotransmitter dopamine. This is logical because medications that increase dopamine are effective treatments for ADHD. Furthermore, brain-imaging studies have identified abnormalities in the dopamine-rich frontal and striatal regions in individuals with ADHD. In animal models used to investigate ADHD, “knock-out” mice—mice missing a gene important for increasing dopamine—are hyperactive and do not respond to stimulant treatment. Their dopamine can not be increased, and they remain hyperactive.
Currently the genes most likely to cause ADHD are thought to involve dopamine regulation. The dopamine transporter (DAT) gene is the prime candidate. This gene regulates the amount of dopamine in the synapse by determining how much dopamine is reabsorbed into the presynaptic neurons. In controls, the dopamine transporter keeps the level of dopamine in the synapse relatively high. In ADHD, the DAT “overfunctions” and lowers the level of synaptic dopamine. Stimulants inhibit DAT. As a result, more dopamine remains in the synapse. Other possible causal genes control postsynaptic dopamine receptors. They affect the sensitivity of the receptors to dopamine. It may take more dopamine to activate the postsynaptic receptors in children with ADHD.
So what does this knowledge mean for treating children with ADHD? First, it may help scientists design better medications for treating ADHD. They can target the cause of the neurotransmitter problem. Second, scientists can work toward treatments, called gene therapy, that correct the genetic abnormalities by replacing the abnormal gene. Gene treatment is currently being tried for a number of serious progressive neurological disorders.
Genetic studies of ADHD have focused largely on genes involved in controlling the neurotransmitter dopamine. This is logical because medications that increase dopamine are effective treatments for ADHD. Furthermore, brain-imaging studies have identified abnormalities in the dopamine-rich frontal and striatal regions in individuals with ADHD. In animal models used to investigate ADHD, “knock-out” mice—mice missing a gene important for increasing dopamine—are hyperactive and do not respond to stimulant treatment. Their dopamine can not be increased, and they remain hyperactive.
Currently the genes most likely to cause ADHD are thought to involve dopamine regulation. The dopamine transporter (DAT) gene is the prime candidate. This gene regulates the amount of dopamine in the synapse by determining how much dopamine is reabsorbed into the presynaptic neurons. In controls, the dopamine transporter keeps the level of dopamine in the synapse relatively high. In ADHD, the DAT “overfunctions” and lowers the level of synaptic dopamine. Stimulants inhibit DAT. As a result, more dopamine remains in the synapse. Other possible causal genes control postsynaptic dopamine receptors. They affect the sensitivity of the receptors to dopamine. It may take more dopamine to activate the postsynaptic receptors in children with ADHD.
So what does this knowledge mean for treating children with ADHD? First, it may help scientists design better medications for treating ADHD. They can target the cause of the neurotransmitter problem. Second, scientists can work toward treatments, called gene therapy, that correct the genetic abnormalities by replacing the abnormal gene. Gene treatment is currently being tried for a number of serious progressive neurological disorders.
Sunday, April 24, 2011
Where in the brain do neurotransmitters have their effects?
Neurotransmitters are chemicals in your brain that pass along information from one cell to another. Neurotransmitters act in the synapse, the space between two brain cells (neurons). Neurotransmitters released by presynaptic neurons act on receptors on postsynaptic neurons (Figure 3). The amount of neurotransmitter in the synaptic space and the sensitivity of the postsynaptic cell receptors determine the neurotransmitter’s effect on the postsynaptic brain cell.
There are many different neurotransmitters. Although dopamine is probably the neurotransmitter that is maximally involved in ADHD, norepinephrine and serotonin probably play lesser roles. The relative balance among these neurotransmitters may be as important as their absolute amounts. Dopamine is the main neurotransmitter in the striatum, while norepinephrine is the main neurotransmitter in the frontal lobe.
There are many different neurotransmitters. Although dopamine is probably the neurotransmitter that is maximally involved in ADHD, norepinephrine and serotonin probably play lesser roles. The relative balance among these neurotransmitters may be as important as their absolute amounts. Dopamine is the main neurotransmitter in the striatum, while norepinephrine is the main neurotransmitter in the frontal lobe.
Saturday, April 23, 2011
What parts of the brain are affected in ADHD?
In studies of ADHD children, the structures that most often have been found to play a role are the frontal lobes, the striatum (particularly the caudate), and the connection between these structures, which is called the frontostriatal circuitry. More recently, the cerebellum has also been found to play a role in ADHD (Figure 1).
If you are not a neurologist, that explanation probably does not mean much, so here is a quick lesson in brain anatomy and function. Your brain is made up of four lobes: frontal, parietal, temporal, and occipital. By and large, the frontal lobes control executive functioning (e.g., planning, organizing, starting, persisting, shifting, and inhibiting impulsive behaviors). The parietal lobes control sensory functions and spatial skills (especially the right parietal lobe). The temporal lobes control language comprehension and memory, and the occipital lobes control vision. The left frontal lobe has the bigger effect on language-related executive functions, and the right frontal lobe has more of an influence on spatial executive function (Figure 2).
The striatum is made up of a number of structures deep within the brain, the caudate being the most active in ADHD. In healthy individuals, the striatum is rich in dopamine. Some structures in the striatum play a significant role in motor function. Parts of the striatum are low in dopamine in such movement disorders as Parkinson’s disease, leading to tremors and very slow movements. Parts of the striatum have also been found to be involved in tic disorders.
The frontostriatal circuitry forms the connection between the frontal lobes and parts of the striatum. Brain cells connect these structures, and the connection is maintained by information passed between the cells via neurotransmitters.
Finally, the cerebellum is part of the hindbrain and has been thought to primarily handle coordination. However, recent studies suggest it plays an important role in cognitive functions, such as language and attention, as well as motor planning. Cerebellar striatal frontal circuitry may also play a role in ADHD.
If you are not a neurologist, that explanation probably does not mean much, so here is a quick lesson in brain anatomy and function. Your brain is made up of four lobes: frontal, parietal, temporal, and occipital. By and large, the frontal lobes control executive functioning (e.g., planning, organizing, starting, persisting, shifting, and inhibiting impulsive behaviors). The parietal lobes control sensory functions and spatial skills (especially the right parietal lobe). The temporal lobes control language comprehension and memory, and the occipital lobes control vision. The left frontal lobe has the bigger effect on language-related executive functions, and the right frontal lobe has more of an influence on spatial executive function (Figure 2).
The striatum is made up of a number of structures deep within the brain, the caudate being the most active in ADHD. In healthy individuals, the striatum is rich in dopamine. Some structures in the striatum play a significant role in motor function. Parts of the striatum are low in dopamine in such movement disorders as Parkinson’s disease, leading to tremors and very slow movements. Parts of the striatum have also been found to be involved in tic disorders.
The frontostriatal circuitry forms the connection between the frontal lobes and parts of the striatum. Brain cells connect these structures, and the connection is maintained by information passed between the cells via neurotransmitters.
Finally, the cerebellum is part of the hindbrain and has been thought to primarily handle coordination. However, recent studies suggest it plays an important role in cognitive functions, such as language and attention, as well as motor planning. Cerebellar striatal frontal circuitry may also play a role in ADHD.
Friday, April 22, 2011
Do children outgrow ADHD?
Many children do outgrow ADHD. However, the latest data suggest that 50% to 70% of children continue to have some symptoms of ADHD in adolescence, and as many as 50% have persistent ADHD in adulthood. However, even in persistent cases, the number of symptoms decrease during adolescence and usually decrease further in adulthood. The types of symptoms also change. Hyperactivity and impulsivity tend to disappear, although adults with ADHD will often comment on their mental as opposed to physical restlessness. From a biological vantage point, the reduction of symptoms probably reflects brain maturation that continues through adolescence and beyond.
Thursday, April 21, 2011
At what age does ADHD most often surface?
The disorder affects individuals of all ages. Of the millions of visits for ADHD to community physicians, about 5% are preschoolers, approximately 66% were elementary school-age, 20% were teenagers, and 15% were adults. ADHD is, however, most often diagnosed in elementary school-age children. Some children are diagnosed later during their junior high school and high school years. It also is not unusual for individuals to receive their first diagnosis of ADHD as adults. Interestingly, many parents first recognize that they have ADHD when it is diagnosed in their child. As this disorder was not diagnosed very frequently years ago, many individuals went through their school years with undiagnosed ADHD. Subsequently, when parents see their children experiencing similar difficulties, they remember their own history, are able to relate, and confirm their own undiagnosed disorder.
ADHD can be diagnosed in preschoolers. Indeed, the peak age of onset, which is different from the age at diagnosis, may be between ages 3 and 4. Not surprisingly, severity affects the age at which ADHD is first noticed, with those more severely affected presenting at a younger age.
ADHD can be diagnosed in preschoolers. Indeed, the peak age of onset, which is different from the age at diagnosis, may be between ages 3 and 4. Not surprisingly, severity affects the age at which ADHD is first noticed, with those more severely affected presenting at a younger age.
Wednesday, April 20, 2011
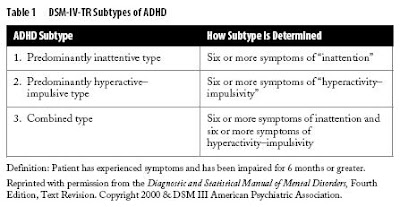
Do different types of ADHD exist?
Yes. The DSM-IV-TR identifies three subtypes of ADHD (Table 1). Some children have symptoms that suggest a mainly hyperactive–impulsive type. To meet criteria for this subtype, a child must exhibit six or more symptoms (including restlessness, frequent interrupting, or talking excessively; see Table 2 for the list of core symptoms). The second subtype emphasizes inattention. To have a diagnosis of this subtype of ADHD, a child must have difficulty following directions, fail to pay close attention to details, be forgetful in daily activities, or become easily distracted. In the third subtype, the combined type, a child must display six or more symptoms of both inattention and of hyperactivity–impulsivity.
Tuesday, April 19, 2011
How common is ADHD?
ADHD is quite common; it is conservatively estimated to affect 3% to 5% of school-age children. Some reports suggest that as many as 4% to 8% or even an amazing 10% to 18% of children have ADHD. Thus, somewhere between 2 and 13 million American children have ADHD. Put another way, on the average, at least one child in every classroom has ADHD. ADHD results in millions of physician visits per year.
Approximately 60% of children with ADHD have symptoms that persist into adulthood. This means that close to 8 million adults (about 4% of the U.S. adult population) have ADHD. However, as ADHD is a behavioral disorder still lacking a specific biological marker, estimates of its frequency can be affected by a number of factors.
The method for making the diagnosis most certainly affects the estimated frequency. The current DSM-IV-TR standards, which allow both hyperactive–impulsive and inattentive subtypes, have resulted in higher rates of diagnosis than previous DSM standards, which placed a higher emphasis on hyperactivity as a diagnostic criterion. In other words, the frequency of the diagnosis increases when hyperactivity is not regarded as a necessary characteristic for ADHD diagnosis. The looser the requirements are, the greater the number of individuals included under the diagnostic umbrella.
The estimated frequency of ADHD also depends on who provides the information to make the diagnosis: parent, teacher, child, or physician. All have their own agendas to report. Teachers are seeing children through the lens of the classroom, where there are specific academic and behavioral expectations. In a class full of children, disruption by a single student can have a ripple effect. On the other hand, in a large class full of children, teachers may not notice the quietly inattentive child. Children may be less aware of their own symptoms. Adolescents, in particular, are notorious for underreporting and minimizing their symptoms. Parents view their children’s behavior from the perspective of day-in, day-out living. Their perspective is intensive as well as long-term. On the one hand, they may minimize symptoms that they have been living with for years. On the other hand, the behavior seen under the intensive lens of daily living may make them keenly aware of things that go unnoticed by others. Physicians see children in a rather artificial setting, where the child is the focus of attention and may be on his or her best behavior. Conversely, some children are stressed by a visit to the doctor and will immediately demonstrate ADHD-like signs by wandering around the office, touching and picking up everything in sight.
Approximately 60% of children with ADHD have symptoms that persist into adulthood. This means that close to 8 million adults (about 4% of the U.S. adult population) have ADHD. However, as ADHD is a behavioral disorder still lacking a specific biological marker, estimates of its frequency can be affected by a number of factors.
The method for making the diagnosis most certainly affects the estimated frequency. The current DSM-IV-TR standards, which allow both hyperactive–impulsive and inattentive subtypes, have resulted in higher rates of diagnosis than previous DSM standards, which placed a higher emphasis on hyperactivity as a diagnostic criterion. In other words, the frequency of the diagnosis increases when hyperactivity is not regarded as a necessary characteristic for ADHD diagnosis. The looser the requirements are, the greater the number of individuals included under the diagnostic umbrella.
The estimated frequency of ADHD also depends on who provides the information to make the diagnosis: parent, teacher, child, or physician. All have their own agendas to report. Teachers are seeing children through the lens of the classroom, where there are specific academic and behavioral expectations. In a class full of children, disruption by a single student can have a ripple effect. On the other hand, in a large class full of children, teachers may not notice the quietly inattentive child. Children may be less aware of their own symptoms. Adolescents, in particular, are notorious for underreporting and minimizing their symptoms. Parents view their children’s behavior from the perspective of day-in, day-out living. Their perspective is intensive as well as long-term. On the one hand, they may minimize symptoms that they have been living with for years. On the other hand, the behavior seen under the intensive lens of daily living may make them keenly aware of things that go unnoticed by others. Physicians see children in a rather artificial setting, where the child is the focus of attention and may be on his or her best behavior. Conversely, some children are stressed by a visit to the doctor and will immediately demonstrate ADHD-like signs by wandering around the office, touching and picking up everything in sight.
Monday, April 18, 2011
Does gender have an effect on ADHD in children?
Most studies indicate that more boys than girls have ADHD. The ratio is probably 2–3:1 in school-age children. One study that researched the frequency of ADHD in school-aged children in the United States found the rate in boys was 9% compared to a rate of 3% in girls. Age seems to have an effect on the gender ratio. The male:female ratio drops in adolescence toward 1:1. In fact, some adult studies even suggest that women have ADHD more often than men. As hyperactivity lessens, the inattentive form of ADHD more commonly seen in girls may persist and equalize the ratio.
Bear in mind, however, that these study results are determined by the detection of ADHD. Gender ratios may be affected by referral practices. Among children referred to child psychiatrists or psychologists, the boy–girl ratio varies from 3:1 to 9:1, whereas in community surveys of school-age children, it is closer to 2:1. More severely or obviously affected children are probably referred to a specialist and are usually boys. It is possible, however, that ADHD goes undetected in girls more often than it does in boys. In this regard, it is important to note that boys and girls tend to have different types of ADHD. Boys more often have the hyperactive–impulsive type or the combined type, whereas girls more often have the inattentive type. Some people suggest that this difference affects the frequency with which ADHD is picked up. In other words, boys could receive diagnoses more often because they are more vocal, their problematic behavior is more obvious, and they are more troublesome for their teachers and families. Although girls tend to be affected less often than are their male peers, some studies suggest that those with diagnosed ADHD tend to be less bright and have more academic difficulties than do boys with ADHD. It is possible that very bright girls simply compensate better and their ADHD goes undetected.
Bear in mind, however, that these study results are determined by the detection of ADHD. Gender ratios may be affected by referral practices. Among children referred to child psychiatrists or psychologists, the boy–girl ratio varies from 3:1 to 9:1, whereas in community surveys of school-age children, it is closer to 2:1. More severely or obviously affected children are probably referred to a specialist and are usually boys. It is possible, however, that ADHD goes undetected in girls more often than it does in boys. In this regard, it is important to note that boys and girls tend to have different types of ADHD. Boys more often have the hyperactive–impulsive type or the combined type, whereas girls more often have the inattentive type. Some people suggest that this difference affects the frequency with which ADHD is picked up. In other words, boys could receive diagnoses more often because they are more vocal, their problematic behavior is more obvious, and they are more troublesome for their teachers and families. Although girls tend to be affected less often than are their male peers, some studies suggest that those with diagnosed ADHD tend to be less bright and have more academic difficulties than do boys with ADHD. It is possible that very bright girls simply compensate better and their ADHD goes undetected.
What is attention deficit hyperactivity disorder (ADHD)?
Attention deficit hyperactivity disorder (ADHD) is a disorder in which a child displays hyperactive, impulsive, and/or inattentive behavior that is age-inappropriate. ADHD is a result of an atypical chemical balance in the brain, which means that ADHD is a physical problem, not an emotional problem. Outside factors, such as poor parenting, a chaotic home situation, divorce, or school stresses may affect how the symptoms come to light, but they do not cause ADHD. In order to diagnose ADHD (according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision [DSM-IV-TR]), problems of inattention and/or hyperactivity and impulsivity must interfere with a child’s functioning in at least two settings (home, school, or social situations). In addition, the guidelines state that at least some symptoms must have been present before the age of 7 years.
Subscribe to:
Comments (Atom)